Claim Submission
Our claim submission services ensure clean, accurate, and timely claims that maximize reimbursements while reducing denials.
Importance of Accurate Claim Submission
Accurate claim submission is critical for healthcare providers to maintain smooth revenue cycles. Even small errors in coding, documentation, or payer rules can result in delays, denials, or revenue loss. We eliminate these challenges with a structured, technology-driven process.
Step 1: Claim Preparation
We carefully compile and verify all claim data — patient demographics, insurance details, and coding accuracy — to ensure claims are clean before submission.
This proactive preparation reduces rejections and accelerates approvals, ensuring providers maintain healthy cash flow.
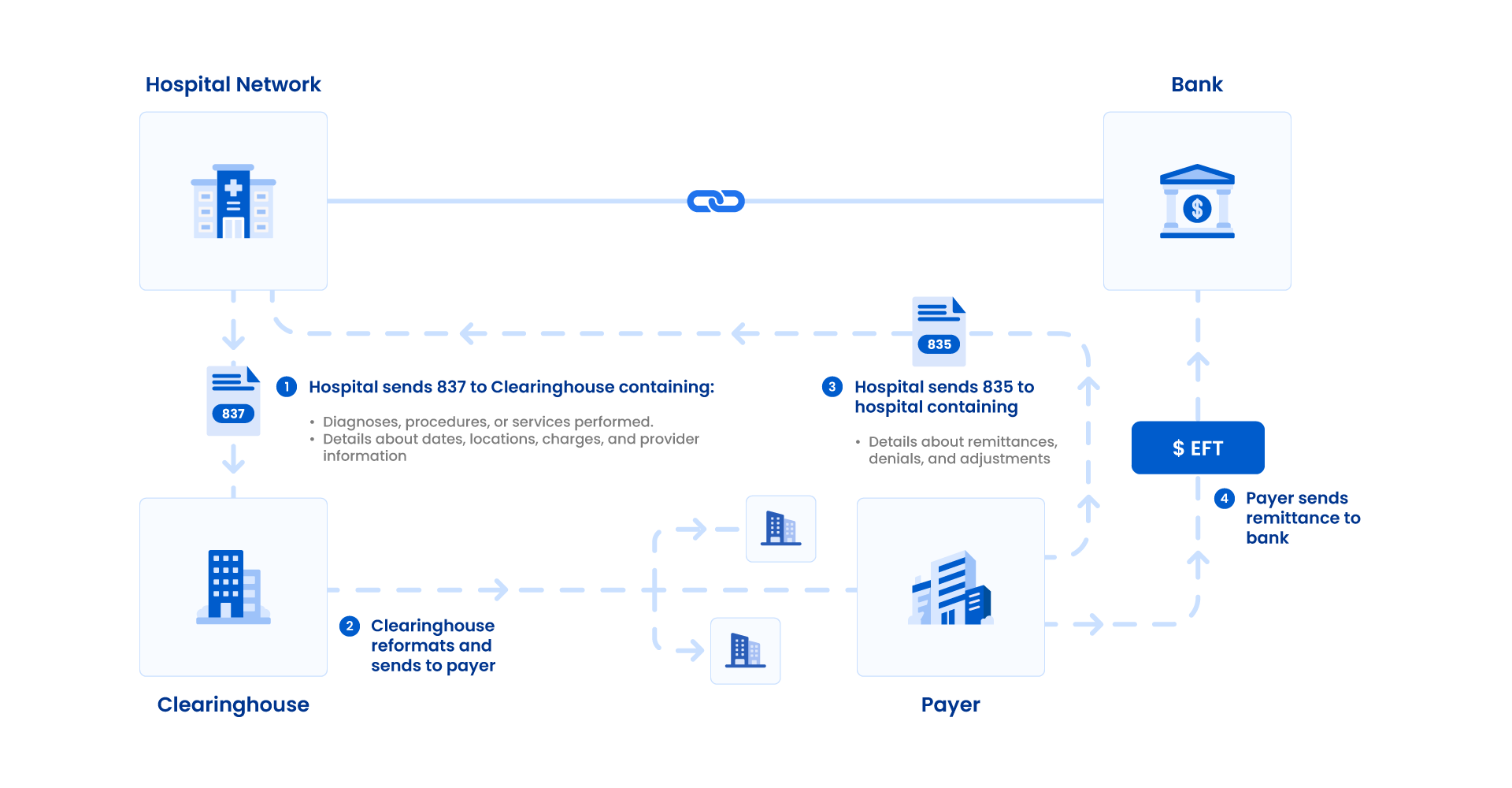
Step 2: Electronic Submission
Claims are transmitted electronically via secure EDI channels, ensuring compliance with payer-specific requirements.
Our process minimizes delays, eliminates manual errors, and speeds up claim settlements.
Our Streamlined Process
Claim Preparation
Gather and validate patient demographics, insurance details, and coding accuracy to prepare claims for submission.
Electronic Submission
Submit claims through secure EDI channels, ensuring they meet payer requirements and clearinghouse validations.
Error Check & Compliance
Run pre-submission audits to identify errors, compliance issues, and coding mismatches before reaching payers.
Tracking & Monitoring
Monitor claim status in real time, quickly identifying rejections and taking corrective actions for faster approvals.
98%
Clean Claim Rate
35%
Reduction in Denials
2 Days
Avg. Turnaround Time